Managing Chronic Achilles Tendinopathy: Latest Advances
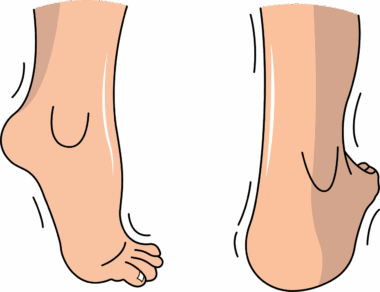
Chronic Achilles tendinopathy (CAT) is a prevalent condition affecting athletes and physically active individuals. It arises from chronic overuse and is characterized by pain, swelling, and functional limitations of the Achilles tendon. Early diagnosis is crucial in managing CAT to avoid long-term complications. Traditional management approaches include rest, ice therapy, and physical therapy. However, new evidence suggests that comprehensive rehabilitation programs are essential for optimal recovery. Incorporating eccentric loading exercises has been found to promote tendon strength and functionality. In addition, adjunct therapies such as shockwave therapy and platelet-rich plasma (PRP) injections are gaining traction as effective treatment modalities. These innovative options aim to accelerate healing by enhancing blood flow and reducing inflammation in the tendon. Understanding the underlying causes of CAT is also vital for developing appropriate interventions. Biomechanical factors, such as foot biomechanics and running gait, can significantly influence tendinopathy development. Early assessment of these factors is instrumental in treatment planning. Interprofessional collaboration among physiotherapists, podiatrists, and sports physicians is essential for implementing tailored rehabilitation protocols. Education about tendon health also plays an important role in long-term management strategies.
Diagnosis and Clinical Assessment
A thorough clinical assessment is pivotal for diagnosing chronic Achilles tendinopathy. Healthcare professionals should conduct a detailed history taking, focusing on the patient’s activity level, symptoms, and previous injuries. Physical examination should assess tendon tenderness, swelling, and range of motion deficits. Special tests, such as the Thompson test and the Royal London Hospital test, can help confirm the diagnosis. Additionally, imaging studies like ultrasound or MRI may be utilized for further evaluation. These tools can provide valuable insights into tendon structure and help rule out other potential injuries. Identifying associated risk factors is also crucial in the diagnostic process. These may include biomechanical issues, pre-existing conditions, and improper footwear. Once diagnosed, an individualized treatment plan should be developed, considering both the severity of the condition and the patient’s specific needs. Patient education is fundamental during this phase, helping individuals understand the nature of their injury and the rationale behind chosen interventions. Rehabilitation should be gradually introduced, ensuring a safe return to activities. Regular follow-ups can help monitor recovery progress and make necessary adjustments to the treatment strategy.
Recent advances in scientific research have significantly influenced the understanding of chronic Achilles tendinopathy. In particular, insights regarding tendon cellular physiology have progressed, leading to innovative treatment protocols. Researchers emphasize the importance of mechanical loading as a stimulus for tendon adaptation. This principle forms the basis for eccentric exercises, which are now a cornerstone in rehabilitation. Emerging studies also discuss the role of bioactive substances in tendon healing processes. Substances like growth factors and cytokines are believed to contribute positively to tissue repair. The interplay between loading and biological activity may provide new avenues for therapeutic interventions. From an exercise perspective, periodization of loading intensity and volume is essential for optimal outcomes. Progressive overload should be incorporated gradually, allowing for tissue adaptation and minimizing re-injury risks. Understanding the patient’s feedback regarding pain levels is key in this approach. With ongoing research, the future of Achilles tendinopathy management looks promising. Advanced imaging techniques and bioanalytical tools will likely aid in personalized treatment decisions. Integrating sports science knowledge with clinical skills is vital for optimizing recovery in individuals suffering from chronic Achilles conditions.
Integrative Treatment Approaches
The management of chronic Achilles tendinopathy increasingly involves integrative treatment approaches. These include combining different modalities to amplify therapeutic outcomes. Alongside exercise therapy, modalities such as transfusion of platelet-rich plasma (PRP) are considered. PRP is derived from the patient’s blood, contains growth factors, and is believed to enhance the healing process. Other alternative options being explored are stem cell therapies, which show promise in regenerating damaged tissues. This suggests a trend toward biological solutions that foster healing at a cellular level. Using modalities like deep oscillation therapy and kinesiology taping can also facilitate pain relief and enhance blood flow around the tendon. Additionally, neuromuscular electrical stimulation (NMES) may further aid in recovery by stimulating muscle contractions. An essential component of integrative approaches is the emphasis on patient-centered care. Patients should be actively involved in their treatment decisions. This empowers them and helps tailor the rehabilitation process to their needs and preferences. Holistic management should also address psychosocial factors impacting recovery, acknowledging that mental health plays a crucial role in the healing journey.
Return-to-sport criteria after an episode of chronic Achilles tendinopathy should be meticulously planned. Establishing specific benchmarks ensures that athletes can return safely to their respective sports. Criteria commonly include pain-free performance, adequate strength testing, and functional assessments. Evaluating the athlete’s ability to manage sport-specific movements is essential. This may include jumping, sprinting, and cutting maneuvers, depending on the sport involved. Once criteria are met, a structured reconditioning phase can begin, progressively introducing sport-related activities. Close monitoring of symptoms and performance during this phase is critical to prevent re-injury. Additionally, education on biomechanics and injury prevention strategies is paramount. Coaches and athletes should collaborate to ensure optimal loading and recovery management during training sessions. Promoting good practices such as proper warm-up and cooldown routines can mitigate the risk of reoccurrence. Strategies should also include attention to footwear selection, as inappropriate shoes might exacerbate chronic issues. Continuous learning about recent findings in sports medicine can empower athletes and coaches alike. Implementing preventive measures alongside rehabilitation can contribute significantly to sustaining long-term tendon health and athletic performance.
Future Directions in Research
As the field of sports medicine continues to evolve, research on chronic Achilles tendinopathy remains a priority. Future studies are expected to explore novel treatment modalities and refine existing management strategies. Promising avenues include investigating genomic and molecular profiling techniques, which could tailor approaches to individual needs based on genetic factors influencing healing. Longitudinal studies analyzing the long-term effects of combined therapies on functional outcomes will also be invaluable. Incorporating qualitative research methods can offer deeper insights into patient experiences and recovery perceptions. Understanding how psychological aspects influence rehabilitation adherence may enhance treatment compliance. Collaborative research efforts involving interdisciplinary teams will be fundamental in advancing knowledge and practice in Achilles pathology. The use of technology, such as wearable devices and telemedicine, is also emerging as promising tools for monitoring rehabilitation outcomes and enhancing communication between patients and providers. Additionally, the ramifications of novel training techniques on tendon health warrant further examination. A comprehensive approach, integrating perspectives from biomechanics, psychology, and tissue engineering, will likely drive important breakthroughs in the management of chronic Achilles tendinopathy.
In conclusion, managing chronic Achilles tendinopathy requires a multifaceted approach that includes advanced treatment modalities, comprehensive rehabilitation programs, and ongoing patient education. Modern strategies must integrate conventional therapies with innovative techniques targeting tissue healing. Continuous engagement with new research findings will help refine management principles and improve patient outcomes. Additionally, an individualized approach to treatment, considering personal factors influencing recovery, will yield better results. By recognizing the significance of biomechanics and psychological health within rehabilitation, healthcare professionals can offer more holistic care. Podiatrists, physiotherapists, and sports physicians must collaborate to optimize patient-centered treatment continuously. Incorporating patient feedback during the recovery process will also support empowerment and adherence. Ultimately, addressing both the physical and psychological aspects of chronic conditions will lead individuals toward successful rehabilitation and return to their active lifestyles. The future of chronic Achilles tendinopathy management looks bright, driven by scientific advancements and an integrative therapeutic approach. With persistent research and innovation, athletes facing this challenging condition can look forward to effective interventions and lasting recovery.