Advancements in Arthroscopic Techniques for Shoulder Injuries
Shoulder injuries can significantly impact an athlete’s performance. Recent developments in arthroscopic techniques have revolutionized orthopedic surgery, enhancing patient outcomes. Arthroscopy is a minimally invasive procedure allowing surgeons to repair damaged tissues using specialized instruments. Compared to traditional procedures, it offers reduced recovery times and minimized complications. Key advancements include the use of high-definition cameras, improved visualization, and innovative surgical tools. These technologies enable surgeons to accurately diagnose and treat various shoulder conditions, including tears of the rotator cuff, glenohumeral instability, and impingement syndromes. Additionally, the transition to arthroscopic techniques has minimized the need for large incisions, improving postoperative comfort for patients. Many athletes can return to their sports more quickly due to the quicker healing associated with this approach. Rehabilitation protocols have also evolved alongside these surgical techniques, focusing on restoring mobility and strength through targeted exercises. Overall, these advancements represent a significant leap forward in sports medicine and orthopedic surgery, ensuring athletes receive state-of-the-art care.
Enhanced Imaging Techniques
Imaging plays a crucial role in diagnosing shoulder injuries. Recent advancements in diagnostic imaging, such as MRI and ultrasound, have greatly improved the accuracy of injury assessment. These improved techniques allow surgeons to visualize soft tissues and bone structures in detail, enabling precise planning for arthroscopic procedures. Enhanced imaging helps identify small tears and lesions that may have been overlooked in the past. As a result, surgeons can develop more effective treatment plans tailored to a patient’s specific condition. Furthermore, the use of 3D imaging technology has gained popularity in preoperative planning. Surgeons can interact with a digital model of the shoulder, leading to superior decision-making during surgery. The prevalence of these imaging modalities has also facilitated better communication between healthcare providers and patients. By sharing detailed images, doctors can educate patients about their injuries, thereby improving trust and compliance. Consequently, enhanced imaging techniques contribute to more successful surgical interventions and rehabilitation outcomes. Overall, the continued evolution of diagnostic imaging in shoulder injuries underscores its significance within orthopedic surgery.
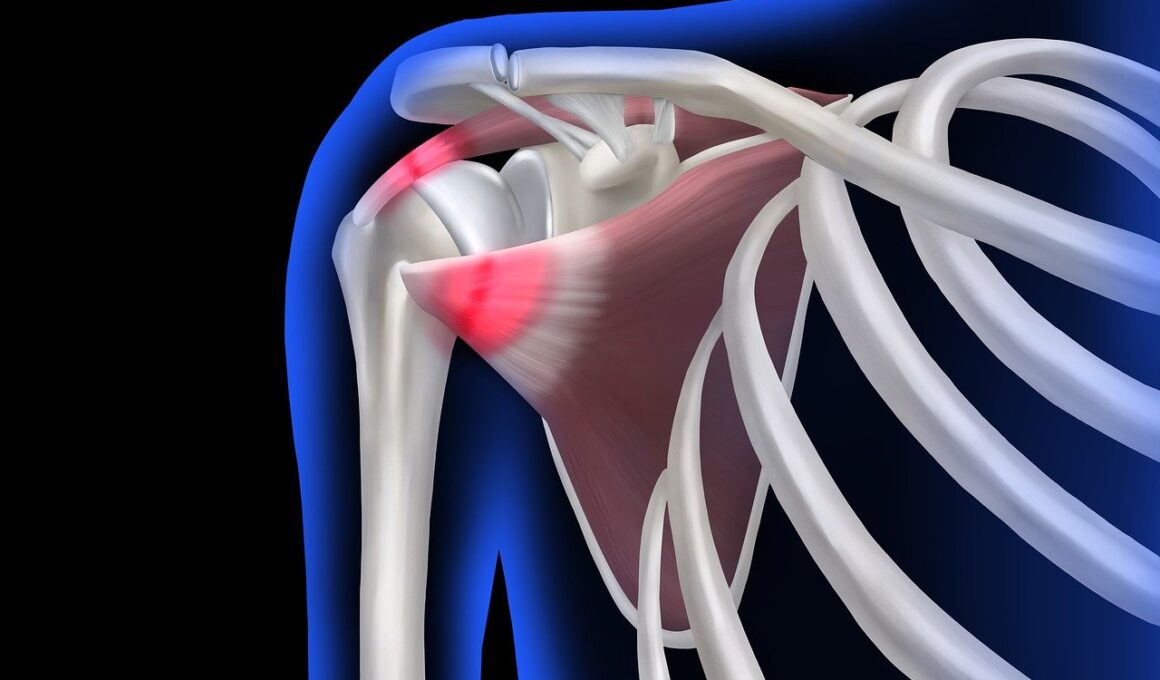
Common shoulder injuries necessitate targeted arthroscopic interventions. Rotator cuff tears are prevalent among athletes involved in overhead sports, often resulting in pain and decreased functionality. Arthroscopic repair typically involves reattaching torn tendons to the bone, and advancements have improved suture techniques. Surgeons now utilize anchors that securely hold sutures, enabling stable joint restoration. This method not only optimizes healing but also preserves shoulder mobility. Another notable condition is shoulder dislocation, where the upper arm bone detaches from the shoulder socket. Arthroscopy allows surgeons to address this issue with minimal tissue damage. Surgeons can use arthroscopic techniques to tighten the shoulder capsule and prevent future dislocations. Moreover, impingement syndrome is effectively treated through arthroscopic decompression, which alleviates pressure on shoulder structures. By removing bone spurs and inflamed tissues, surgeons can enhance joint function and reduce discomfort. Each of these treatments showcases how arthroscopic advancements in orthopedic surgery directly improve the quality of life for athletes and active individuals alike.
Postoperative Rehabilitation Innovations
Rehabilitation plays a crucial role following arthroscopic shoulder surgery. The recovery phase emphasizes restoring mobility, strength, and stability to the shoulder joint. Recent trends include the incorporation of physical therapy protocols that are minimally invasive while also promoting active healing. Such protocols eliminate stiffness and enhance overall function. Additionally, the progression of rehabilitation exercises is carefully monitored to ensure optimal recovery times, thereby allowing athletes to return to their sports more effectively. Recent advancements in technology have also introduced remote therapeutic interventions whereby physical therapists can guide patients through virtual sessions. This approach helps maintain patient engagement and adherence to therapy schedules. Furthermore, the use of wearable technology in rehabilitation programs enables real-time compliance tracking. These innovations allow for personalized adjustments based on patient performance. Consequently, athletes receive targeted therapies that cater to individual needs, ultimately translating to better outcomes. Overall, the evolution of postoperative rehabilitation practices ensures athletes effectively regain their peak performance post-surgery, demonstrating the cyclical nature of advancements in arthroscopic surgery.
Research continues into the long-term outcomes of arthroscopic procedures for shoulder injuries. Studies reveal that the overall satisfaction rates among patients remain high, with many reporting significant improvements in pain levels and functionality. This is largely due to the combination of advanced surgical techniques and enhanced postoperative care. Moreover, the precise nature of arthroscopic surgery results in minimized scarring and complications, resulting in a more favorable recovery experience. Longitudinal studies have also examined the efficacy of various rehabilitation protocols, reinforcing that early initiation of rehabilitation contributes to better outcomes. Continued tracking of these patients signifies a commitment to refining surgical practices and postoperative strategies. Furthermore, the inclusion of patient feedback provides valuable insights into their experiences, further informing the orthopedic community’s approach to shoulder injuries. By prioritizing patient-centered care, researchers strive to elevate standards in orthopedic surgery globally. Consequently, these efforts consolidate the positive impact of recent advancements, emphasizing that patient satisfaction remains the ultimate goal in arthroscopic shoulder injury treatments.
The Role of Biologic Augmentation
Manufacturers have explored biologic augmentation in arthroscopic shoulder surgeries. Techniques such as the application of platelet-rich plasma (PRP) and stem cell therapies are being integrated to enhance healing. These biologic treatments aim to utilize the body’s healing mechanisms to improve surgical outcomes. PRP involves collecting a patient’s blood, processing it to concentrate the platelets, and injecting it into the surgical site. This accelerates tendon healing and reduces inflammation, showing promise in shoulder repairs. Stem cell therapies, meanwhile, harness the body’s regenerative capabilities to repair damaged tissues. Research into the efficacy of these therapies continues to expand, with preliminary studies yielding positive results. These biologic advancements may play a crucial role in the future of orthopedic surgery, particularly for patients hesitant or unable to undergo traditional invasive procedures. By focusing on natural healing, providers are optimizing post-surgical recovery while minimizing the risk of complications. As these trends advance, orthopedic surgeons must remain well-versed in both traditional surgical techniques and innovative biologic therapies.
The integration of robotic-assisted surgery represents one of the latest advancements in arthroscopic techniques. Robotic systems provide enhanced dexterity and precision during surgeries, allowing surgeons greater control over their instruments. This capability is particularly beneficial in complex shoulder reconstructions where detailed manipulation is essential. The technology facilitates a superior level of surgical accuracy, which translates to improved outcomes and potentially shorter recovery times for patients. Currently, robotic-assisted procedures are in various stages of implementation, continually evolving to meet the specific demands of different arthroscopic applications. Coupled with high-definition imaging technology, robotic systems enable surgeons to visualize anatomical structures more clearly than ever before. This clarity enhances decision-making during critical phases of surgery, ensuring patients receive the best possible care. Professional education on robotic surgery is becoming essential for orthopedic surgeons, as this technology evolves. As robots become more prevalent within arthroscopic surgery, their use may redefine industry standards. Ultimately, these advancements promise a future where shoulder injury treatments are more effective and efficient, offering compelling opportunities for both patients and healthcare providers.
Conclusion
In summary, the evolution of arthroscopic techniques for shoulder injuries has transformed orthopedic surgery. Enhanced imaging, innovative surgical approaches, and postoperative rehabilitation advancements all contribute to improved patient outcomes. Furthermore, research into biologic augmentation and robotic-assisted surgery signifies the future direction of sports medicine. As these technologies continue to develop, a greater understanding of their effects will drive further improvements in treatment methodologies. Ongoing education for healthcare professionals is essential to adapt to these advancements continually. By focusing on patient-centered care and exploring new technologies, orthopedic surgeons can enhance the quality of treatment. As a result, athletes can return swiftly to their sports, regaining vital functionality while minimizing complications. The end goal is to foster a health-oriented environment where patients experience optimal recovery from shoulder injuries. Continuous collaboration within the medical community will ensure the integration of best practices in this evolving field. The advancements seen today promise even better outcomes for the athletes of tomorrow, illustrating the dynamic nature of orthopedic care in the context of sports medicine.